On this page, I will share special cases and experiences from the hospital. New entries will appear from time to time throughout my stay, so feel free to check back.
Every day at the hospital brings something new. Today, our primary focus was assembling an emergency box for life-threatening postpartum hemorrhage. This condition can occur when the uterus fails to contract properly, leaving blood vessels in the uterine wall uncompressed. It's particularly common after a cesarean section since contractions during surgery aren't as strong as in natural childbirth. Thankfully, it doesn't happen often, but when it does, quick action is crucial. Our emergency box includes IV fluids, medications like tranexamic acid to aid blood clotting, and essential supplies such as gloves, intravenous catheters, and disinfectants. The goal is to have everything readily available at the scene to provide immediate assistance. Postpartum bleeding is a life-threatening condition. On our way to the Maternity Ward , we meet Nurse Heriett and explain our emergency box to her. She assures us that she will inform all the obstetricians at the hospital about it.
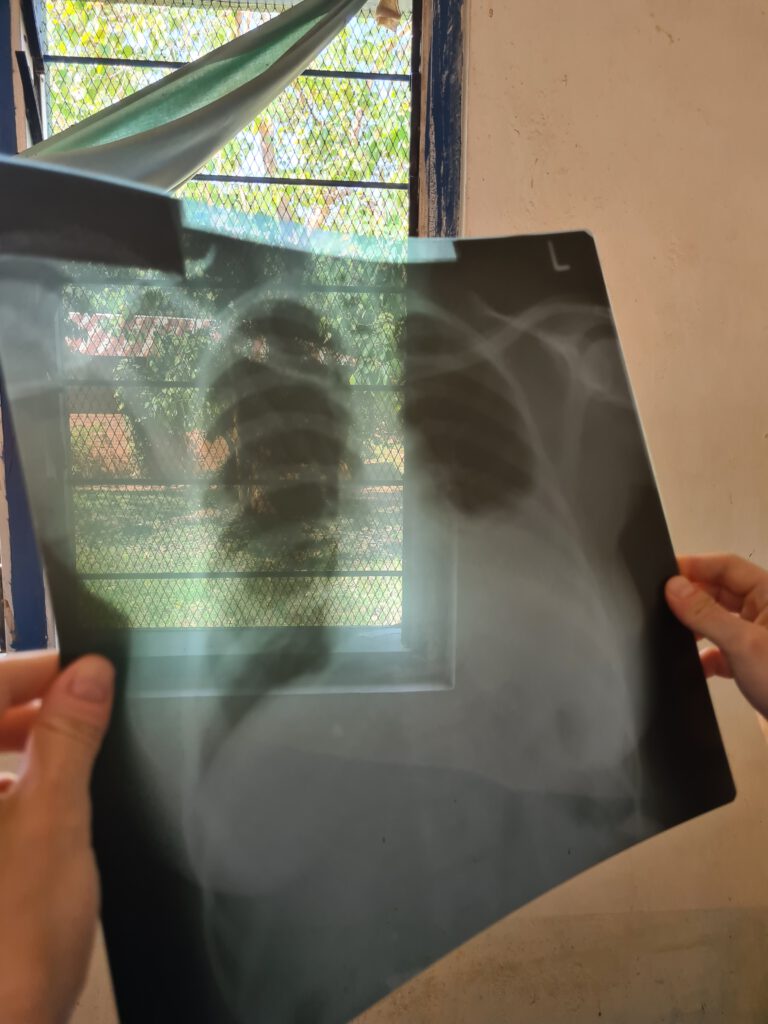
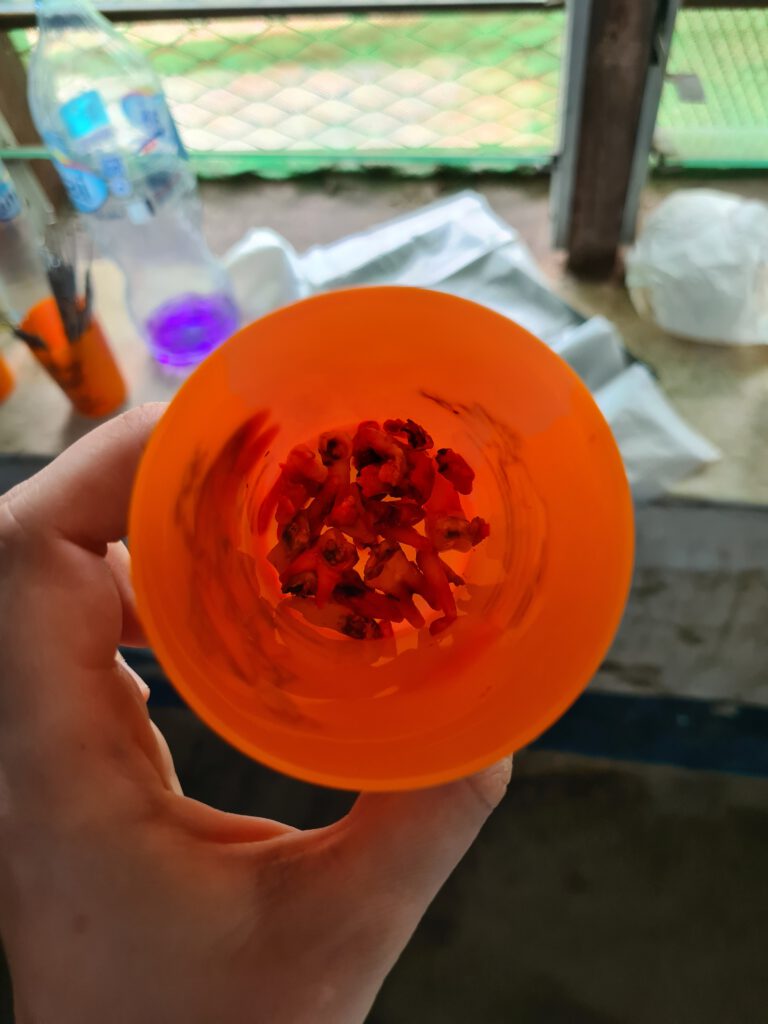
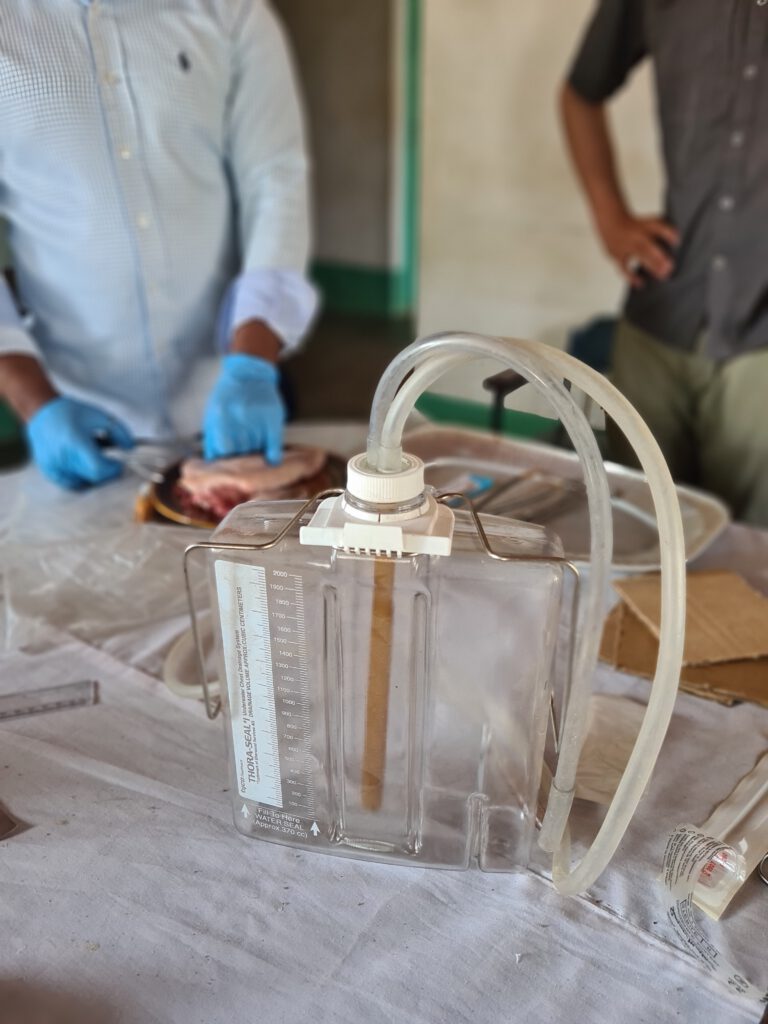
Now, let me share the story of a patient who came to us with chest pain after falling on her left side three days ago. She had visible bruises over her lower left ribs, and the area was tender to touch. Such chest trauma requires a detailed assessment of nearby organs, particularly the lungs and the spleen, located in the upper left abdomen. Using a stethoscope, we note weakened breath sounds in the lower left lung, suggesting the presence of fluid—possibly blood—instead of air. Next, we examine the abdomen clinically and perform an ultrasound to rule out a ruptured spleen or internal bleeding in the abdominal cavity. The abdominal ultrasound is unremarkable, but when we examine the lungs, we detect fluid accumulation even with the patient lying down. Dr. Evans orders a standing Chest X-Ray , which confirms the presence of a hematoma in the left chest cavity—a condition known as a hematothorax. Tim and I agree that the woman urgently needs a chest drain to remove the blood and prevent potential infection. Left untreated, such infections can lead to severe complications. Tim offers to place the drainage tube himself, as the two local doctors lack experience with this procedure. However, there is no chest drainage system available, and they are hesitant to improvise one. Instead, they decide to transfer the patient to Songea, a journey that will take several hours by bus. We hope she reaches safely and receives the necessary treatment. Following this case, Tim adds a chest drainage set to our list of essential supplies, and the two Tanzanian doctors are enthusiastic about the idea of a future Teachings on this procedure.

The other day in the OPDA woman came to the Outpatient Department (OPD) complaining of pain and restricted movement in her right elbow joint following a fall onto her outstretched hand. After a brief clinical examination, I suspected that the bone wasn’t broken but the joint was possibly dislocated and needed to be repositioned. Unfortunately, the X-ray film had run out, leaving us unable to confirm whether a fracture was present. This was not only a significant setback for the hospital but also a challenge for the patient. A fracture must be ruled out before attempting a manual reduction of a joint. Lacking alternatives, we explained the situation to the patient and discussed the risks and benefits of proceeding with the reduction. We also talked about the use of anesthesia to minimize her discomfort. Tim and I proposed administering a low dose of intravenous ketamine, a painkiller commonly used in Liuli for general anesthesia but not in sub-anesthetic doses. After preparing a body weight-adapted dilution of ketamine in a 5 ml syringe, we administered it incrementally, reaching a total of 40 mg. This effectively controlled her pain. Dr. Evans then performed the reduction maneuver. While the nurse stabilized the upper arm, Dr. Evans applied traction to the forearm and performed a twisting motion. Within seconds, the joint slid back into place. The patient, slightly groggy from the ketamine, was allowed to rest, and her arm was placed in a sling for the next few days. Later that afternoon, the anesthesia nurse visited us at the Doctors House terrace, eager to learn more about this application of ketamine. I explained it to her step by step and wrote down the dosage and dilution details for her to share with her colleagues and display in the Minor theatre .
Today, a 46-year-old, emaciated woman comes to our Outpatient DepartmentShe complains of having lost an incredible 34 kg in five months! Her current weight is now more like 36 kg. We delve deeper into her medical history and find out that she also has occasional episodes of fever. An HIV test was negative. She also complains of pain in her lower right abdomen. The physical examination reveals a clearly noticeable resistance in the right lower abdomen, or in other words: a tumor. Not good at all. We recommend an ultrasound, which can only be carried out once the patient's financial resources have been clarified. At the same time, a blood count is taken, which shows pronounced anemia. When we hold the transducer to the abdomen, a mass is clearly visible, most likely from the internal genitals or intestines. In view of the rapid weight loss and anemia, everything points to an advanced stage of cancer. Dr. Evans gently explains this suspicion to the patient. It is clear that she cannot be adequately cared for in Liuli. We recommend that she be seen in Peramiho or Songea, where there is at least the possibility of surgical resection and histological analysis. Complementary cancer treatment (chemotherapy or radiotherapy) is only available in Tanzania in Dar Es Salaam. However, as with all uninsured Tanzanians, it is unfortunately also a question of money for this patient as to how intensive the therapy will be.
A True Rarity
Two new volunteers arrive today: Barbara, a newly qualified doctor and emergency paramedic, and Moritz, an emergency paramedic and physiotherapy student. Knowing that there is no physiotherapist in Liuli, I identify a few patients last week who might benefit from physiotherapy—those with chronic musculoskeletal pain or injuries. Moritz’s arrival sparks the idea of organizing a crash course in physiotherapy for one or two hospital staff members during his stay. I immediately think of Mr. Richard, the enthusiastic radiology technician who greets everyone with a cheerful Mambo poa – Poa Poa and a fist bump. Since the X-ray machine is currently out of operation due to a lack of films, Mr. Richard has some extra time on his hands. When I suggest the training, he is very interested. I hope that with Moritz’s help, we can introduce basic physiotherapy knowledge and skills in Liuli, laying the groundwork for better care in the future.
Dental Volunteers
The Dental Volunteers have now arrived in Liuli. We are cooperating with this non-profit organization from Germany for the first time this year. To put it simply, dental care in Liuli has been non-existent until now. The general rule is that broken teeth are simply pulled. Consequential diseases such as malnutrition, abscesses and blood poisoning, heart and vascular diseases are treated as best as possible with the resources of St. Anne's Hospital. At the end of 2022, however, something happens: the Tanzanian government provides the hospital with a Dental Therapist . However, she remained unemployed initially due to the absence of dental equipment in Liuli. Recognizing the urgent need for proper dental care, the Bishop of Ruvuma and the Hospital Secretary brought this situation to our attention. We planned to invest in a complete Dental Unit, which will be put into operation at the beginning of 2023. Patients with dental problems can now also be treated in Liuli. But that's not all, we are now welcoming the Dental Volunteers to Liuli. Over the next few weeks, they will be visiting the surrounding schools and communities to offer free on-site treatment. Patients with serious problems can be referred to St. Anne's Hospital if necessary. The offer is very gratefully accepted by the pupils and residents of the Nyasa Districts . As the Dental Volunteers are self-organized, we can simply take part in the implementation of their project and are delighted with another successful measure to improve healthcare in Liuli.


The new disease
One of the buildings on the hospital grounds has so far remained hidden from me: the HIV outpatient clinic. It is a little way away from the other buildings. Today, Tim and I stop by because people from a Tanzanian organization that collects data on HIV in Tanzania are there. Curious as Tim is, he squeezes the guests thoroughly. HIV prevalence in the Nyasa District is above the national average. Knowledge about the disease and the risk of transmission is very rudimentary among young people, which leads to many new infections, especially in this age group. I spontaneously come up with the idea of initiating a project in which volunteers visit all the surrounding Secondary Schools , establish awareness-raising lessons there and perhaps also distribute condoms. Incidentally, these are free in Tanzania. The same goes for pre- and post-exposure prophylaxis, which should be taken before or after potentially infectious contact. Otherwise, we learn from the Data Scientiststhat the adherence of HIV patients to treatment is very high. Treatment is fully paid for by the government, which is why the dropout rate is very low. At the same time, I am told that the topic of HIV is rather frowned upon by society. I have noticed that the doctors in Liuli often talk about „the new disease“ in front of patients.
We are constantly sending students and medical staff from all kinds of professions to Liuli. We are very pleased about your interest in the topic and would be happy to discuss the possibilities of a project to improve HIV awareness!


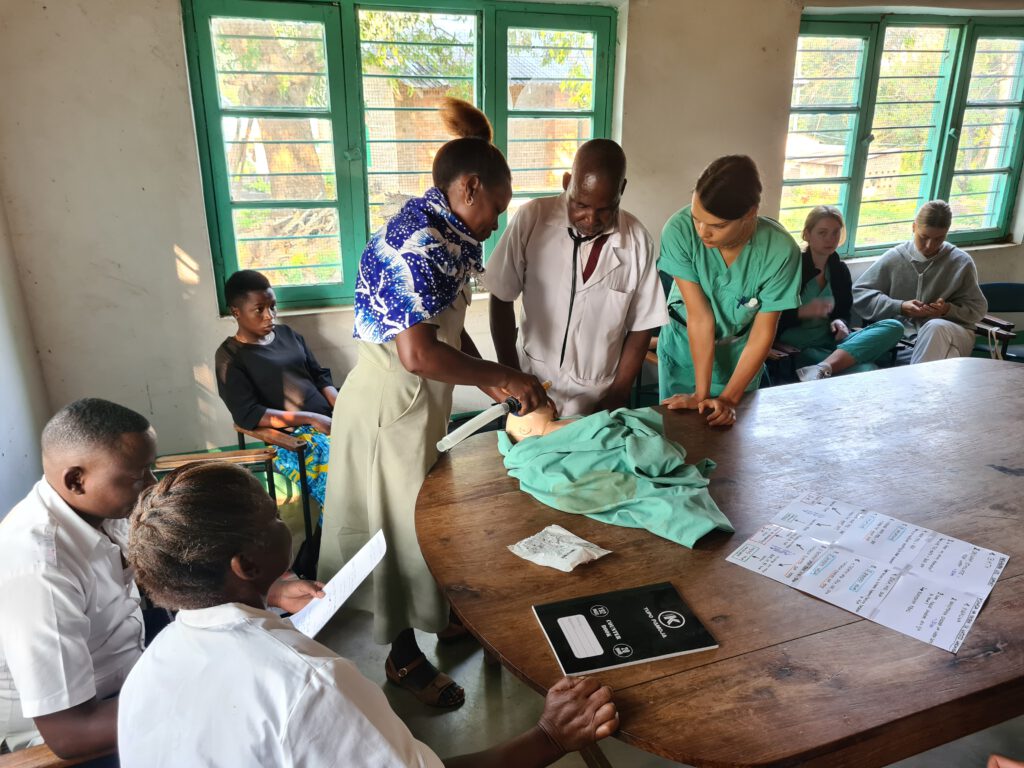
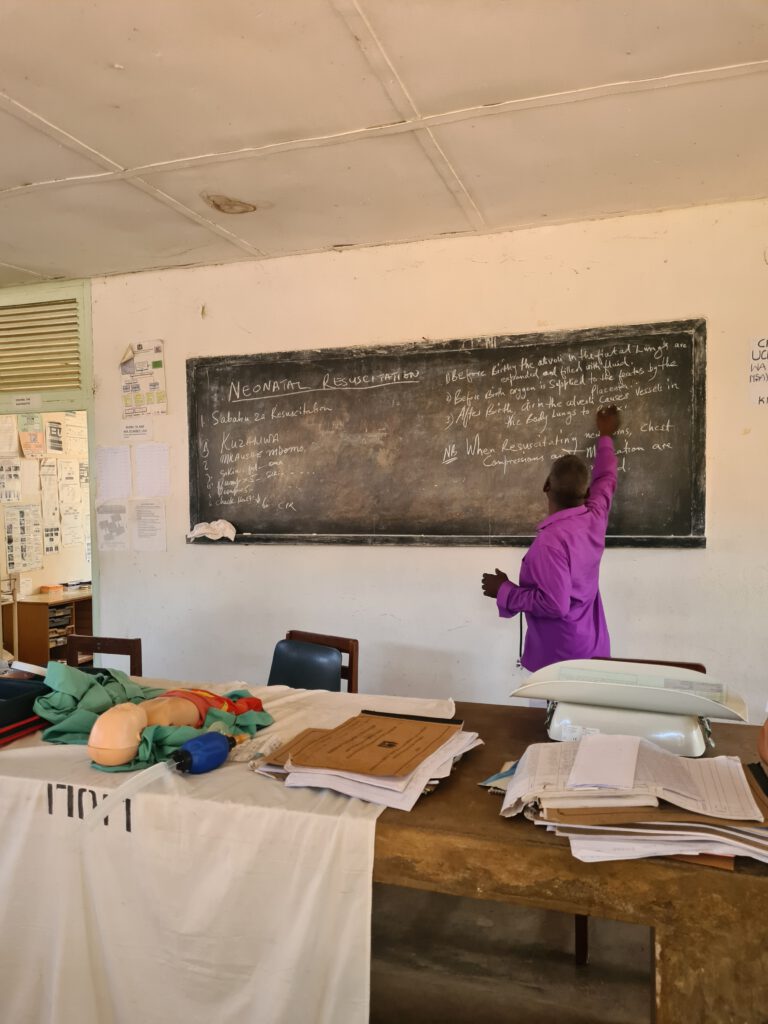
Newborn resuscitation training
Newborn resuscitation training is taking place at St. Anne's Hospital this week. Babsi and Moritz, who both trained as emergency paramedics before studying medicine and physiotherapy respectively, are designing a training session for the hospital staff and all volunteers together with the highly interested and very experienced anesthesia technician Mr. Bernard. What may sound like a niche skill to many at first glance is in fact far too often the brutal reality at St. Anne's Hospital. Many newborns require ventilation and sometimes circulatory support immediately after birth. Why is that? The caesarean section rate here last year was around 43%. In Liuli, this means that 43% of newborns are born under the influence of the anesthetic drug Ketanest. Ketanest is an established emergency and anesthetic drug in many countries around the world, as it not only relieves pain but also has a sedative effect without impairing the protective reflexes (e.g. breathing reflex, swallowing reflex, cough reflex). The latter is a huge advantage over other anesthetic drugs, because when using Ketanest there is no need to secure the mother's airway or ventilate her. Unfortunately, however, the child receives a good dose of Ketanest via the umbilical cord vessels. In addition, most caesarean sections are performed here for high-risk pregnancies with birth complications. After birth, the children are therefore often very limp and their breathing sluggish. To reduce infant mortality, it is therefore very important to provide regular training in neonatal resuscitation in order to be prepared in the event of an emergency. Previously, staff had to travel to Mbinga, a long way away, for such training. Thanks to the new training manikin and Mr. Bernard, Babsi and Moritz, the training can now be offered directly at St. Anne's Hospital at regular intervals. A flow chart with the most important steps will be displayed in the operating and delivery rooms.

Water March
Today, Tim and I are shown the pump that pumps water from Lake Nyasa to the hospital. It is located in a small bay not far from the stretch of beach where Doctors House is situated. Together with the Hospital Secretary and the Plumbing, we climb into a very wobbly rowing boat, which tips dangerously to one side if we suddenly shift our weight. The water level in the boat remains constant at around 5 cm, although Tim diligently skims off the water with a small canister. The others are not worried at all. We only drive about 20 meters out onto the lake until we see the pump shimmering through the clear water. Today the filter that protects the water pipe from the mud in the lake is to be replaced. The plumber jumps off the boat and gets to work, and after several attempts he finally succeeds. We also learn that the pump is solar-powered. For technical reasons, however, the solar system cannot be fitted with a battery, so it can only be pumped when the sun is shining. On cloudy days and at night, the hospital therefore has to rely on expensive water from the Tanzanian government or run the pump with a diesel (and money) consuming generator. In response to our queries, we are told that a pump with a higher output would be necessary to cover the demand at night and even to accumulate a certain supply in the tank. When it comes to the association's investments, we generally give higher priority to projects that have a direct impact on patient care. Since I've been here, however, I've become increasingly aware that in order to maintain and improve care, the hospital must first keep its head above water - in the truest sense of the word.


Sometimes it is very quiet at St. Anne's Hospital, and then suddenly so much happens at once.
First, the hospital secretary is stung several times by a wasp-like insect. The right side of his face swells up and he develops wheals on his upper arms and thighs. In an emergency, he is given a cortisone preparation intravenously and adrenaline intramuscularly. Fortunately, he got better quickly and his breathing was never impaired. However, he has definitely had a big scare.
Then a 60-year-old woman is admitted with right-sided facial paralysis, gaze turned to the right and severe clouding of consciousness. Urgent suspected diagnosis: stroke. We would actually like to know whether the cause is a cerebral hemorrhage or a vascular blockage, but of course we don't have a CT scan here. Besides, our room for maneuver is very limited anyway. I know from Dr. Evans that strokes are treated here with an oral cholesterol-lowering drug. After three days, aspirin is added. A sugary solution can be administered intravenously to reduce intracranial pressure. In this case, the stroke is probably triggered by a blood pressure derailment. The automatic measuring device aborts the measurement and with the manual device I pump the cuff up to over 280 millimeters of mercury only to find that the blood pressure is apparently even higher. Unfortunately, the only emergency antihypertensive medication available here is only available as a tablet, which we cannot administer orally due to the woman's state of consciousness. We administer the tablet rectally and also try to insert a feeding tube - unfortunately without success. We noticed repeated seizures in her right hand, which we treated with an antiepileptic drug. On the evening of the day she was admitted, the woman died.
The only local doctor present is required in the operating room at the same time. He performs a caesarean section on a woman who has been in labor for two days. When the baby is born, it appears completely limp and is not breathing. After suctioning and a few initial ventilations with the bag, it finally begins to breathe on its own and the bluish-grey color of the skin gives way to a healthier color. Nevertheless, the child made an extremely strained and weak impression. We first hand it over to the grandmother in a stable condition, as the mother is still weak from the operation, which fortunately went without any further complications for her.
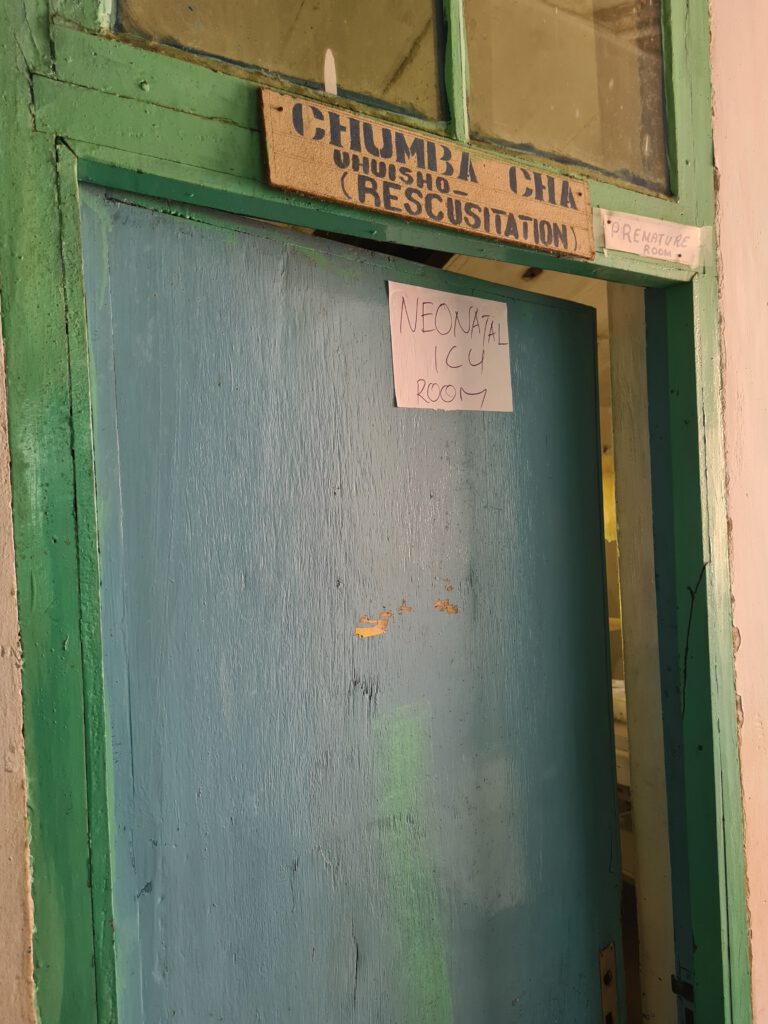
When we check on the little girl the next morning, her respiratory rate has risen sharply and she has developed a fever. We take the child to the neonatal intensive care unit - it's just a table with a heat lamp, but it's not working at the moment. We give oxygen via an oxygen concentrator because the saturation in the blood is far too low. Due to the language barrier, it is difficult to determine whether the child has already drunk - probably not. We feed the girl first with a sugar solution via a nasal feeding tube, then with some breast milk and finally with a mixed formula milk and electrolyte solution. Due to the accelerated breathing and the fever, the little girl has a significantly increased need for calories and fluids. I can see from her wrinkled skin that she is clearly in a fluid deficit. The attempt to insert a vascular access fails several times. I get some paracetamol syrup from the pharmacy for the fever. We assume the most likely scenario is pneumonia due to aspiration of stool or early onset neonatal sepsis (blood poisoning). In the absence of a vascular access, we have to administer the antibiotics in small doses intramuscularly and orally via the feeding tube. To make matters worse, the baby has had a complicated birth. In the worst case scenario, she has suffered brain damage due to a lack of oxygen. At regular intervals, her muscle tone is greatly increased and her eyes move rapidly back and forth, which we call nystagmus. The grandmother is very concerned about her granddaughter and often comes to see us when we check on her. She also asks us questions directly, which is actually rather unusual in my experience so far. We can also communicate reasonably well in Swahili. She tells me that the little girl's name is Antonia (with an accent on the "i"). The mother, who is only 16 years old, seems very apathetic to me. I would like to ask her how she is doing and whether there is anything we can do for her.
One of us checks on Antonia every two hours during the night. It's my turn at 11 pm and 5 am. I have the impression that her skin looks less dry now, but the girl is still breathing very quickly and her fever only drops towards the end of the night. In the end, her body temperature is even below 36°C despite the warm blankets. At 7 a.m., the oxygen machine fails once, whereupon Antonia's heart stops beating for about two minutes. But then she comes back again. At the next visit, we give her antibiotics again and her mother gives her some breast milk. However, Antonia becomes weaker and weaker and eventually her heart only beats 36 times a minute. As a result, her organs are no longer supplied with sufficient oxygen. We ask the obstetrician to bring the mother and grandmother into the room. The grandmother wants to hold Antonia again. We withdraw to give them some privacy. I don't know the exact time of death.


My blog has become a little quieter. That's because we're working a lot at the moment. Patient care is one thing, but we also want to push ahead with our association projects while we're here. For example, the X-ray room needs better radiation insulation and the electricity system urgently needs an overhaul - there are currently no fuse boxes or lightning conductors in the hospital buildings. Some washbasins and pipes need replacing. But we are also pushing ahead with our medical projects. Every Wednesday, we conduct neonatal resuscitation training for nursing staff and obstetricians. When we arrive late at the hospital on a Wednesday, they even call us and ask for the training. I am extremely pleased that our offer is so well received. The topic of newborn care has been on my mind a lot since we lost little Antonia. In the same week, we resuscitated a small premature baby in the 30th week of pregnancy several times, in the end without success. Another baby died during a nocturnal birth that we were not called to. All in all, it was a very sad week. I drew conclusions from my experiences. There is now an emergency kit in both the operating room and the delivery room, equipped with a resuscitation bag and mask for newborns, manual throat suction, stethoscope and pulse oximeter, among other things. I also set up a new neonatal intensive care unit. Previously, this was simply a small room with a defective warming unit. Now there is also an emergency kit here with all the necessary examination items. There is also an oxygen machine, hot water bottles, feeding tubes, formula nutrition, which I found when I was clearing out the pharmacy, and much more. Notes on the walls explain in English and Swahili what a sick newborn needs. I created a provisional ICU-chart (ICU = intensive care unitin Excel, in which the vital parameters as well as clinical examination results and medication administered are entered. I collected most of the equipment at the hospital - it was all there, just not in the right place. But a sick newborn needs help quickly.



Tunasafiri Ng’ombo
Today Tim and I are traveling with the hospital secretary to Ng'ombo [Nombo] to a dispensary. Dispensaries are small health centers in particularly remote places without hospital connections. The care is mainly outpatient, but there are also a few beds for inpatients. The reason for the visit is originally an administrative act, but Tim and I naturally don't pass up the opportunity for a short trip. My first impression is that it's very idyllic here. There is even a bright pink tree blooming right at the entrance - a color I rarely see in Tanzanian vegetation. We receive a very warm welcome and extremely tasty food. When the first patients arrive, I am soon back in work mode. The noise caused by the chickens in the courtyard of the Dispensarys - and unfortunately also in the consultation room from time to time - takes some getting used to. Tim almost goes into a rage at some point because one of the chickens keeps finding its way into our room. It's mainly children who come to the consultation today with their parents. They all complain of diarrhea and repeated vomiting. After the third child, the nursing staff put on face masks and aprons. I hope there isn't an outbreak of cholera here, I think to myself. The mother of an affected child carries the sick boy's little sibling in a sling on her back. Only the feet and arms are sticking out, but that's enough to attract my attention, because a rash is clearly visible on the skin. When the child sticks its head out of the cloth, it also shows a crust around its mouth and nose. Hand-foot-and-mouth disease is my first association. We ask the mother to undress the child and examine it completely. The rash also extends to the thighs, buttocks, arms, neck and ear. Purpura Schoenlein-Henoch, I think next because of the morphology of the rash, and ask if the child has been ill in the last few weeks. The mother answers in the affirmative, but the little one is now doing excellently again. PSH is an inflammation of the blood vessels that can occur in children after harmless infections, for example of the upper respiratory tract. The course of the disease is usually mild and does not require treatment, so I am not worried about the child who is free of symptoms.



Thoracic Drainage Training
Today we are organizing a chest drainage training course together with our medical colleagues from St. Anne's Hospital. A chest drain is actually a very simple system consisting of a tube, the tip of which is inserted into the chest cavity and the end of which is connected to a plastic canister filled with water. Such a system is required if there is blood or air in the chest cavity. Although air can escape from the lungs via a tube extending into the water (air bubbles visible), the water prevents air from entering the patient via the tube. In addition to air, blood can also be evacuated from the chest cavity through the thick tube. Attentive and loyal readers of my blog will now remember the patient with a haematothorax (blood in the chest cavity), who we unfortunately had to transfer because there was no option for a chest tube at the time. However, we now have an emergency kit with all the important materials for the next patient. Each of us successfully applies a chest tube to the pig model. Before today, I had only been able to do this twice on patients. Since every doctor should be able to do this procedure in an emergency, it is important to practice the moves from time to time.


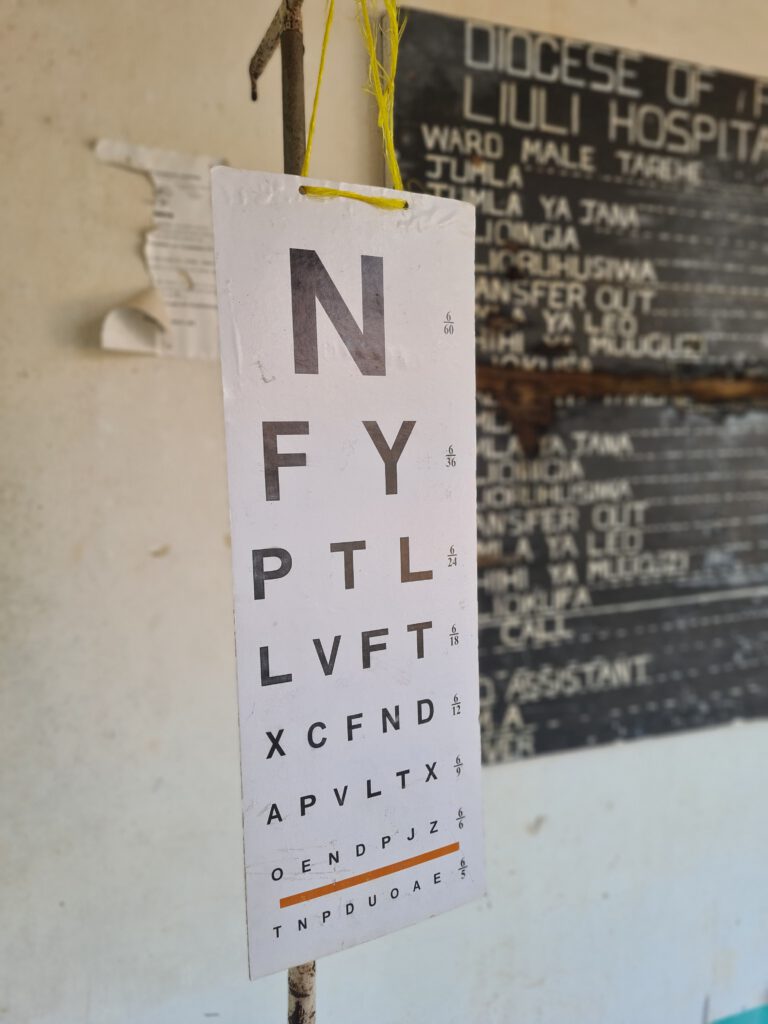
Specialist medical support for Liuli
My last week in Liuli begins. And it is a special week, because the ophthalmologist Dr. Hinju is visiting St. Anne's Hospital. Eye diseases are also very common in Tanzania. In stark contrast to this is the complete lack of ophthalmologic care in the Nyasa DistrictThis is Dr. Hinju's first visit to St. Anne’s, but hopefully not the last. As a rule, the hospital cannot afford specialist medical care - a major problem, the consequences of which we feel every working day here. Be it the 72-year-old man who has gone completely blind over the last few months due to a cataract. Or the young man with knee pain after a motorcycle accident who needs orthopaedic and trauma surgery. To make matters worse, the accident occurs when the hospital does not have enough money to buy new X-ray films. Or the 68-year-old woman with weight loss and a hardening of the right lower abdomen that has been increasing for months, who actually needs a gynecological examination and a colonoscopy (suspected diagnosis: cancer!). Or the 40-year-old woman with a stomach haemorrhage who absolutely needs a colonoscopy and probably an operation to prevent her from dying as a result of anaemia. The premature baby, whose lungs are not yet fully developed, also needs specialized care in order to survive the premature birth. The Hospital Secretary dreams of St. Anne’s becoming an extended care hospital with specialist centers. I would very much like this for the people here, but the road there is still long and arduous.